How Bad Is A Vaginal Hysterectomy With Bladder Repair?

Vaginal Hysterectomy for Prolapse
In this Health Topic
Prolapse is the loss of normal support of the vagina and/or uterus (womb). Prolapse of the uterus and/or vaginal walls is a common condition with up to eleven% of women requiring surgery during their lifetime. Prolapse generally occurs due to damage to the supporting structures of the uterus or vagina. Weakening of the supports can occur during childbirth, following chronic heavy lifting or straining (e.m. with constipation), chronic cough, obesity, and as part of the crumbling process. In some cases, there may be a genetic weakness of the supportive tissues.
Prolapse of the uterus tin can cause an uncomfortable bulging sensation, a feeling of fullness, or pressure in the vagina. In more than advanced prolapse the neck can extend beyond the archway to the vagina.
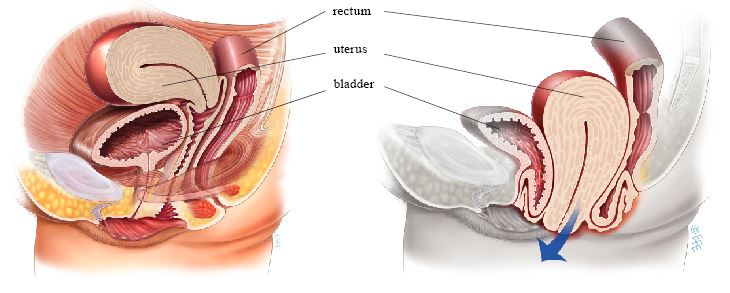
Normal uterus and vagina, no prolapse (left), and Prolapse of the uterus, bladder, and rectum (bowel) (right)
This is a process in which the uterus is surgically removed through the vagina. The operation is frequently combined with prolapse repairs of the bladder and/or bowel. There are no abdominal or laparoscopic incisions.
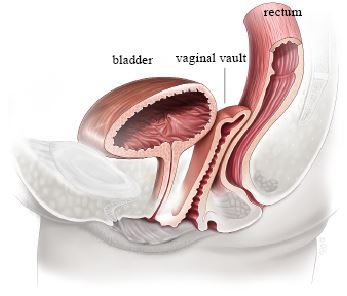
Advent afterward hysterectomy
A vaginal hysterectomy offers many benefits over abdominal or laparoscopic procedures. It offers overall fewer complications, shorter healing time, less pain, less scarring, a lower chance of infection, less risk of hernias, and faster render to activities. Besides, a prolapsed uterus is easier to access via the vagina.
The operation is performed in a infirmary setting and tin be performed under general or spinal anesthesia (with or without sedation). A cut is fabricated around the neck. The surgeon then carefully pushes the bowel and bladder abroad from the uterus. The claret vessels supplying the uterus and surrounding tissue are then clamped and secured. Later on confirming in that location is no haemorrhage, the surgeon removes the uterus and closes the top of the vagina, now known as the vaginal vault.
Many surgeons will choose to add additional support stitches to the vaginal vault at the fourth dimension of surgery – either to the uterosacral ligaments that support the uterus (this is called a uterosacral ligament suspension) or to support structures on the side of the uterus (this is chosen a sacrospinous ligament suspension or ileococcygeus intermission). Leaflets are available on both of these procedures for more than data. These additional stitches help to reduce the risk of the vaginal vault prolapsing in the future. Your doctor tin explicate what he/she plans to do. The ovaries tin be removed during a vaginal hysterectomy if needed.
You will exist asked virtually your general wellness, by medical history and any medication that you are taking. Any necessary tests (for example blood tests, ECG, chest Ten –ray) will be arranged. You will also receive information about your admission, hospital stay, operation and pre- also as mail service-operative care. Mention to your doctor if yous are on blood thinning agents such as aspirin, equally these tin lead to an increased risk of bleeding and bruising during and after surgery. Your md may ask you to stop the claret thinning medications 7 to 10 days prior to surgery. Some surgeons recommend bowel grooming prior to surgery.
When you wake upwards you will accept a drip (IV) to requite y'all fluids and you may have a catheter in your bladder. You may have a vaginal pack to reduce the hazard of haemorrhage. By and large, the pack, catheter, and drip are removed in the get-go 24 to 48 hours after surgery. In most cases you lot will be able to eat and drink most immediately later surgery. Pain and anti-nausea medication are given when needed, either intravenously, by intramuscular injection, or pill.
Keeping mobile after surgery is of import to reduce complications such every bit clots in the legs and breathing problems, including pneumonia. Walking and light household duties are fine, withal heavy lifting (more than 10kgs/25lbs) is not advisable in the first 6 weeks postal service-operatively. It is normal to feel tired following surgery so make sure you schedule rest times in the first few weeks after surgery.
You can expect to stay in the hospital 1-3 days. It is normal to get a creamy/brown or bloody belch for 4 – 6 weeks subsequently surgery. This is due to the presence of stitches in the vagina. As the stitches absorb, the discharge will gradually reduce.
85% of women having a vaginal hysterectomy for uterine prolapse are cured permanently. Nearly 15% of women develop a further prolapse of the vaginal vault months or years later their starting time surgery. These figures may vary depending on the severity of your original prolapse.
With any operation there is e'er a chance of complications:
- Anesthetic problems. With modern anesthetics and monitoring equipment complications due to anesthesia are very rare.
- Clots (embolism). Afterward any pelvic surgery clots can class in the legs or lungs. This is a rare complexity which is minimized by using support stockings and possibly blood thinning agents postal service-operatively (if indicated).
- Severe blood loss and hematoma. The risk of claret loss requiring blood transfusion is small-scale (0-10%) and will in part vary on what other surgery you are having. Virtually ten% of women develop a small drove of blood at the vaginal vault (a hematoma). This normally drains spontaneously subsequently seven to 10 days. Occasionally it will crave surgical drainage.
- Infections. Although antibiotics are given merely earlier surgery and all attempts are made to proceed surgery sterile, at that place is a small gamble of developing a vaginal or pelvic infection. This volition usually present with an unpleasant smelling vaginal discharge and/or fever.
- Urinary tract infection. 6-xx% of women having vaginal surgery develop a urinary tract infection. The take chances is highest if you accept had a catheter. Symptoms include burning and stinging when passing urine and frequency. If yous think you have an infection afterward surgery contact your doctor.
- Injury to adjacent organs. Upward to 2% of vaginal hysterectomies are complicated past either damage to the bladder, the ureters, or rectum. A very rare complication is the occurrence of a vaginal fistula.
- Urinary retention. In the start few days after surgery, difficulty passing urine tin can occur in up to 10-fifteen% of cases. You may need to have a catheter for a few days after surgery until you lot are able to hands pass urine.
- Urinary incontinence. Prior to surgery, it is possible to have had urinary incontinence which was "occult" or hidden by the prolapse. During surgery, the urethra (the tube which empties the float) becomes unkinked or unobstructed, resulting in urinary incontinence becoming obvious mail-operatively. This can occur in 40-45% of cases.
You should exist able to bulldoze and be fit enough for calorie-free activities such as short walks within a few weeks of surgery. You are advised to avoid heavy lifting and sport for at to the lowest degree 6 weeks to let the wounds to heal. Information technology is unremarkably advisable to plan to accept two to vi weeks off piece of work, depending on the type of surgery you have had and the blazon of work yous do. Sex can usually be safely resumed after 6 weeks.
Source: https://www.yourpelvicfloor.org/conditions/vaginal-hysterectomy-for-prolapse/
Posted by: englandhimespeof.blogspot.com


0 Response to "How Bad Is A Vaginal Hysterectomy With Bladder Repair?"
Post a Comment